Is Cervical Disk Replacement Right for You? Exploring the Options
If you’re dealing with cervical disk issues and contemplating surgery, knowing about cervical disk replacement is essential. This article delves into why this procedure is necessary, the various types of artificial disks utilized, eligible candidates, and symptoms and risks to be aware of. Discover the distinctions between this and fusion surgery, explore options, and prepare for the journey ahead.
What is Cervical Disk Replacement?
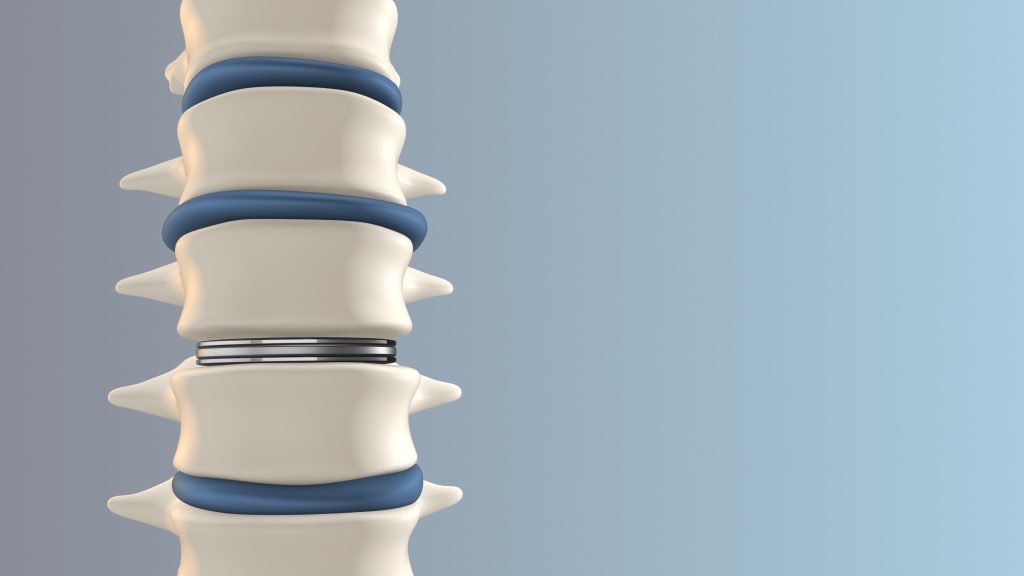
Cervical Disk Replacement, or cervical arthroplasty, involves replacing a damaged cervical disc with an artificial one to restore the natural function of spinal motion segments. It’s performed to address degenerative disc diseases causing neck pain and limited mobility.
The surgery aims to alleviate pain, prevent adjacent segment degeneration, and restore proper alignment and functionality in the neck region by replacing the damaged disc. This procedure offers long-term relief and reduces the risk of further complications associated with degenerative disc diseases.
Who is a Candidate for Cervical Disk Replacement?
A comprehensive evaluation involving multiple disciplines is necessary to assess a patient’s suitability for cervical disc replacement surgery. Age, medical history, overall health, and lifestyle are crucial considerations. The severity of symptoms, spinal instability, and previous surgeries also influence candidacy.
A thorough risk assessment is vital to anticipate potential complications and ensure successful outcomes. The long-term effectiveness and durability of the procedure are significant considerations. A multidisciplinary team, including orthopedic surgeons, neurosurgeons, physiotherapists, and pain specialists, collaborates to provide a holistic evaluation and make informed decisions for the patient’s well-being.
What are the Symptoms of Cervical Disk Problems?
Cervical Disc problems often manifest as persistent neck pain, which can be a sign of degenerative disc disease. Chronic pain in the neck region is a common symptom that indicates potential issues with cervical discs. Individuals with cervical disc problems may experience numbness or tingling in their arms or hands. This radiating discomfort can often be traced back to nerve compression caused by the degeneration of the discs in the neck.
Early detection of these symptoms is crucial as they can progress and lead to more severe complications, such as muscle weakness or difficulty performing everyday tasks. Seeking professional medical guidance to diagnose and treat cervical disc issues properly is essential in managing and alleviating these distressing symptoms.
Types of Cervical Disk Replacement
Exploring the types of cervical disk replacement involves understanding the different artificial disks used in surgery. Each offers specific advantages and disadvantages that impact patient outcomes and recovery.
Common types include metal-on-polyethylene, providing durability but susceptible to wear and tear; ball-and-socket, offering natural motion but with a risk of dislocation; and silicone, known for flexibility and shock absorption but requiring careful consideration due to individual needs and goals.
These disks enhance spinal mobility and functionality, preserve biomechanics, reduce adjacent segment degeneration, and improve post-surgery outcomes. Patients should discuss this option with their healthcare providers to determine the most suitable choice.
Preparing for Cervical Disk Replacement Surgery
Preparing for cervical disk replacement surgery involves undergoing essential preoperative tests and evaluations to ensure readiness for the procedure. These include diagnostic tests like X-rays and MRIs to assess health status and identify potential risks. Meeting with an anesthesiologist to discuss anesthesia options is also crucial.
Patients should be aware of medications to avoid before surgery, such as NSAIDs and blood thinners, to minimize complications. Diligently following pre-operative instructions, including fasting before surgery, is essential for a smooth surgical process and optimal recovery outcomes.
Frequently Asked Questions
1. Is cervical disk replacement the best option for me?
The decision to undergo Cervical Disk Replacement can vary depending on individual health and medical history. It is essential to consult with your doctor to determine if this is the right option for you.
2. How does cervical disk replacement compare to other treatments?
Cervical Disk Replacement is a relatively new procedure and has shown promising results for patients. However, discussing all available treatment options with your doctor is essential to determine which one is best for you.
3. What are the potential risks and complications of cervical disk replacement?
As with any surgical procedure, cervical disk replacement has risks and potential complications. These may include infection, nerve damage, device failure, and others. Discussing these with your doctor and weighing them against the procedure’s potential benefits is essential.
4. How long is the recovery time for cervical disk replacement?
Recovery time can vary depending on the individual and the extent of the procedure. However, most patients can expect to return to normal activities within weeks to months following the surgery.
5. Does insurance cover cervical disk replacement?
In most cases, Cervical Disk Replacement is covered by insurance. However, it is always best to check with your specific insurance provider to determine coverage and any potential out-of-pocket costs.
6. What can I expect during the cervical disk replacement procedure?
During the procedure, a small incision will be made in the neck to access the damaged disc. The damaged disc will then be removed and replaced with an artificial disc. The entire procedure typically takes 1-2 hours and is performed under general anesthesia.
Warning: urlencode() expects parameter 1 to be string, array given in /www/wwwroot/surgeryconsultantsofflorida.com/wp-includes/formatting.php on line 5693

